Most people know that malnutrition is prevalent in developing countries, but most don’t realize malnutrition is also common among the elderly in the United States. This is a growing problem, as the Census Bureau predicts there will be 92 million people over age 65 by 2060. Malnutrition in our elderly population is a serious issue, due to the associated adverse outcomes.
The causes are multifactorial, but studies have shown nutrition care leads to better outcomes and saves money.At-risk individuals that receive nutrition care during and after a hospitalization are 3 times less likely to die.1
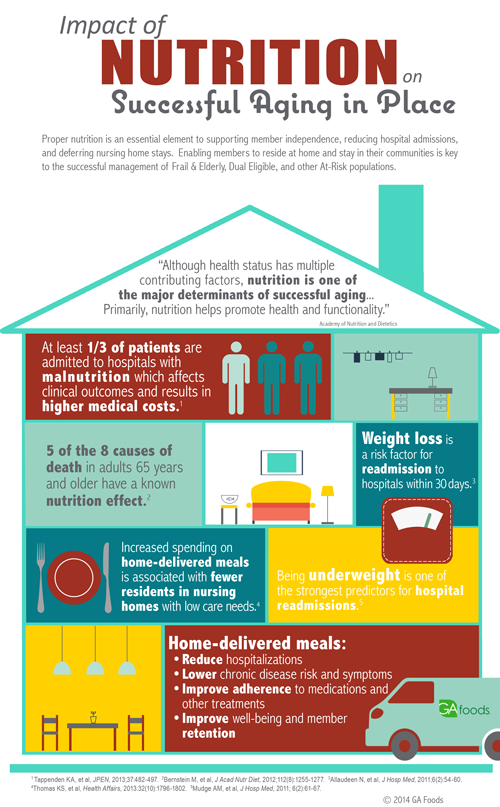
 Individuals with weight loss are at a higher risk for avoidable hospital readmissions. The greater the weight loss, the greater the probability of readmission.3
Individuals with weight loss are at a higher risk for avoidable hospital readmissions. The greater the weight loss, the greater the probability of readmission.3
Malnourished patients have 2-3 times more complications than those not at risk for malnutrition.4
Malnutrition was found in 1/3 of inpatients and resulted in poor hospitalization outcomes and survival.5
59% percent of patients identified with malnutrition risk, were unable to be discharged home with self-care.6
Hospitalized patients discharged with malnutrition are older and sicker. Their inpatient care was 2 ½ times more expensive than those without malnutrition.7
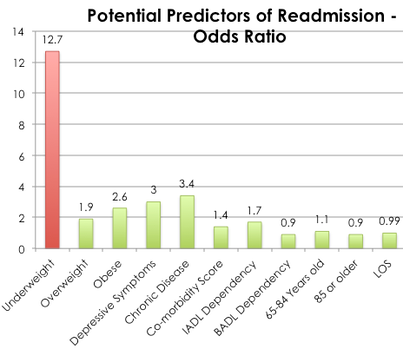
Being underweight is the strongest predictor for hospital readmissions.8
1 Feldblum I, et al, J Am Geriatr Soc, 2011;59(1):10-17.
2 Barker LA, et al, Int J Environ Res Public Health, 2011;8(2):514-527.
3 Friedman JM, et al, Am J Clin Nutr, 1997;65(6):1714-1720.
4 Sorenson J, et al, Clin Nutr, 2008;27(3)340-349.
5 Lim SL, et al, Clin Nutr, 2012;31(3):345-350.
6 Chima C, et al, JADA, 1997;97(9):975-978.
7 Corkins, MR, et al, JPEN, 2014;38(2):186-195.
8 Mudge AM, et al, J Hosp Med, 2011;6(2):61-67.
9 FMQAI, Florida’s Medicare Quality Improvement Organization, under contract with CMS.