
Food Insecurity in the United States
In the US, 48.1 million people live in households with food insecurity - meaning they do not have access to enough food for an active, healthy life. Of those people, 20% or 9.6 million are seniors. Seniors with food insecurity tend to have more medical and mobility challenges. Older adults above the poverty level can also be at risk for food insecurity, particularly if they are unable to shop for and prepare foods.
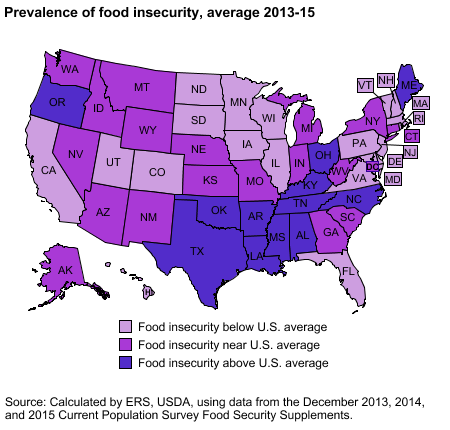
Many confuse food insecurity with hunger, but food insecurity is a social, cultural or economic status, while hunger is a physiological condition – the physical pain and discomfort someone experiences. Hunger doesn’t describe the scope of food insecurity. The scope is more than most realize. Here is a breakdown by state:
In the News - Clarence Blackmon
One example of food insecurity is the story about Clarence Blackmon. Mr. Blackmon, age 81, was discharged from a rehab facility where he had spent many months battling cancer. When he returned to his apartment, his refrigerator was empty. He had money to pay for food, but not enough strength to shop for or prepare food. He didn't have any family in the area. Not knowing what to do, he called 911 and asked the dispatcher to bring him food. The dispatcher brought him food and even made him sandwiches for several meals. Unfortunately, many senior adults experience food insecurity after a hospitalization.
Food Insecurity after a Hospitalization
Food insecurity also has an impact on hospital readmissions. One study interviewed 40 adults with three or more hospitalizations within a 12-month period. They found, that like Clarence, 75% were unable to shop for their own food and 58% were unable to prepare their own food.
Last fall, the Food Forum of the National Academies of Sciences, Engineering, and Medicine held a workshop on Nutrition Across the Life Span for Healthy Aging. One of the presenters, Mary Ann Johnson, emphasized the need to think about nutrition interventions when someone is discharged from a hospital and sent home without meal support. Many end up in acute or long-term care. She “mentioned an ongoing national conversation on how the medical health and social services health systems can work together and suggested that meals are an important link between the two.”
After a hospitalization, patients generally have decreased energy, pain, weakness, and a poor appetite, putting those with food insecurity at an even greater risk for malnutrition, and associated poor outcomes.
Meal Services after a Hospitalization
Connecting food insecure patients with resources such as home-delivered meals (HDM), decreases their need for shopping and cooking after a hospitalization. HDMs provide a regular source of nutritious food for those that need it for their recovery, reducing medical costs and the risk of a hospital readmission.
Many Medicare Advantage health plans, provide post-discharge meals for members after a hospitalization. Members who receive home-delivered meals after a hospital stay regain their strength and energy faster.
To learn more about nutrition care after a hospitalization, download our free white paper:











